Know About Reverse Shoulder Replacement Surgery by Dr. Chintan Desai
Reverse Shoulder Replacement is a specialized joint replacement surgery where the normal anatomy of the shoulder is reversed - the ball and socket switch places.
- In this procedure, a metal ball is placed on the shoulder blade (glenoid), and a plastic socket is fixed at the top of the upper arm bone (humerus).
- This reversal allows the deltoid muscle (instead of the damaged rotator cuff) to power arm movements.
- The surgery is typically recommended when rotator cuff tendons are torn beyond repair or have failed previous surgeries.
- It provides pain relief, restores arm function, and improves stability, especially in patients with rotator cuff arthropathy.
- Reverse shoulder arthroplasty is considered a highly successful option for restoring upper limb function when other treatments don't work.
Who Are the Candidates for a Reverse Shoulder Replacement?

- Patients with massive rotator cuff tears that cannot be repaired are the primary candidates for this surgery.
- It's often suitable for those with arthritis combined with rotator cuff deficiency - also known as cuff tear arthropathy.
- Patients who have undergone a failed previous shoulder surgery, like a standard total shoulder replacement, may benefit.
- Individuals with complex fractures of the shoulder in elderly patients with poor bone quality can be treated using this technique.
- Those experiencing chronic shoulder instability, pain, and poor range of motion due to muscle weakness are considered ideal candidates.
- Generally, it is offered to patients above 65 years of age, but younger patients may be considered based on case severity.
Indications for Reverse Shoulder Replacement
- Irreparable Rotator Cuff Tear: When tendons are so damaged that they can't be reattached or regenerated with physiotherapy.
- Cuff Tear Arthropathy: A condition combining arthritis and torn rotator cuff, leading to joint damage and dysfunction.
- Severe Shoulder Arthritis with Muscle Weakness: In such cases, traditional shoulder replacement won't work effectively.
- Complex Proximal Humerus Fractures: Especially in elderly patients with osteoporosis or multiple fragment fractures.
- Failed Previous Shoulder Surgery: If a standard total shoulder replacement didn't relieve symptoms or caused complications.
- Tumor Resections in the Shoulder Area: Where structural joint reconstruction is needed post-tumor removal.
Possible Complications of Reverse Shoulder Replacement
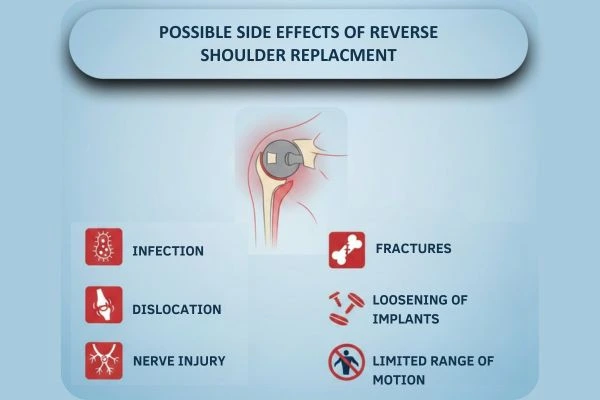
- Infection: As with any major surgery, infection around the implant site is a risk, though relatively rare.
- Dislocation: There is a chance of the artificial joint becoming unstable or dislocating post-surgery.
- Nerve Injury: The brachial plexus and other surrounding nerves can be damaged during surgery.
- Fractures: The humerus or scapula may fracture during implant placement, particularly in osteoporotic patients.
- Loosening of Implants: Over time, the artificial components can wear out or loosen, especially with high activity levels.
- Limited Range of Motion: Although function usually improves, some patients may experience less flexibility than expected.
Pre-Operative Care for Reverse Shoulder Replacement
- Medical Evaluation: A thorough assessment including X-rays, MRI, and blood tests to determine surgical readiness.
- Discussion of Medications: Blood thinners or anti-inflammatory medications may be paused before surgery.
- Anesthesia Planning: Patients will typically undergo general anesthesia; some may receive a nerve block for pain control.
- Prehabilitation: Gentle exercises to maintain existing shoulder mobility and strength before surgery.
- Infection Control: Showering with antiseptic soap and following fasting instructions is often advised.
- Consent and Planning: Detailed discussion with the surgeon about the procedure, risks, and realistic expectations is crucial.
Post-Operative Care After Reverse Shoulder Replacement
- Hospital Stay: Most patients stay in the hospital for 1–3 days following surgery for monitoring and initial rehab.
- Wound Care: Dressings are kept clean and dry; stitches or staples are removed within 10–14 days.
- Pain Management: Medications and nerve blocks help manage early post-surgical discomfort.
- Arm Support: A sling or immobilizer is used to support the arm and protect the new joint during early healing.
- Infection Monitoring: Patients are advised to watch for signs like fever, redness, or discharge at the incision site.
- Follow-Up Visits: Regular check-ups and X-rays are necessary to monitor joint positioning and healing progress.
Rehabilitation After Reverse Shoulder Replacement
- Phase 1: Passive Motion (Week 1–6): Focus on gentle, assisted movements guided by a physiotherapist to avoid stiffness. No active lifting or overhead use of the arm is allowed at this stage.
- Phase 2: Active Motion (Week 6–12): Patients gradually begin moving their shoulder independently. Light stretching and range-of-motion exercises are introduced.
- Phase 3: Strengthening (3–6 Months): Resistance bands and light weights are used to build shoulder and arm muscle strength. Emphasis is on regaining daily activity functions like dressing and reaching.
- Return to Normal Activities: Most patients resume routine work and light activity within 3 months. Full strength and flexibility can take up to 6–12 months depending on age and overall health.
- Lifelong Maintenance: Periodic physiotherapy sessions and home exercises help maintain joint function long term. Avoid high-impact sports or heavy lifting to protect the artificial joint.
Why Choose Reverse Shoulder Replacement? - Key Benefits
- Pain Relief: One of the most consistent outcomes; most patients experience dramatic reduction in pain.
- Improved Arm Function: Even in cases of complete rotator cuff failure, the arm can regain lifting ability.
- Restored Independence: Patients can perform daily activities like dressing, cooking, and grooming with minimal discomfort.
- Enhanced Shoulder Stability: Reversing the mechanics of the joint compensates for lost tendon support and increases joint control.
- Long-Term Results: Modern implants offer good durability, with many lasting 15–20 years.
- Improved Quality of Life: Patients enjoy better sleep, better mood, and a more active lifestyle after recovery.
For expert care, consult Dr. Desai, the best Shoulder Surgeon and Sports Injuries Specialist in Mumbai.
Struggling with shoulder pain? Contact us to Book an appointment today and get back to a pain-free, active lifestyle!
FAQs on Reverse Shoulder Replacement Surgery in Mumbai
How long does reverse shoulder replacement surgery take?
The surgery usually takes around 1.5 to 2 hours.
Is physiotherapy needed after the surgery?
Yes. Physiotherapy is important to regain strength and improve shoulder movement.
Does reverse shoulder replacement reduces pain?
Yes. Most patients experience significant pain relief after the surgery.
When can I return to daily activities?
Most patients can start light daily activities within a few weeks.
Is reverse shoulder replacement suitable for elderly patients?
Yes. It is commonly performed in older patients and helps improve comfort and independence.

About The Shoulder
- Muscles
- Shoulder Conditions
- Shoulder Replacement Surgery
- Reverse Shoulder Replacement
- Shoulder Instability
- Frozen Shoulder Treatment
- Shoulder Impingement Treatment
- Rotator Cuff Tear Treatment
- Arthroscopic Shoulder Surgeries
- Slap (Superior Labrum Anterior To Posterior) Tears
- Latarjet & Remplissage Surgery
- Shoulder Arthritis Treatment
- Calcific Tendonitis
- Examination

Quick Contact Here
+91 22 23062035
022 - 23012732

Watch Our Video