About The Shoulder
- Muscles
- Shoulder Conditions
- Shoulder Replacement Surgery
- Reverse Shoulder Replacement
- Shoulder Instability
- Frozen Shoulder Treatment
- Shoulder Impingement Treatment
- Rotator Cuff Tear Treatment
- Arthroscopic Shoulder Surgeries
- Slap (Superior Labrum Anterior To Posterior) Tears
- Latarjet & Remplissage Surgery
- Shoulder Arthritis Treatment
- Calcific Tendonitis
- Examination

Quick Contact Here
+91 22 23062035
022 - 23012732

Watch Our Video

Know About Shoulder Replacement Surgery by Dr. Chintan Desai
Introduction of Shoulder Replacement Surgery
- Shoulder Replacement Surgery is a modern surgical procedure to relieve pain and restore mobility in severely damaged shoulder joints.
- It involves replacing the damaged parts of the shoulder - typically the ball (humeral head) and sometimes the socket (glenoid) with artificial components.
- This surgery is often recommended when non-surgical treatments like medication, therapy, or injections fail to offer relief.
- Common causes that lead to this surgery include arthritis, fractures, or rotator cuff tears causing persistent pain and stiffness.
- Shoulder replacement can significantly improve quality of life by reducing pain and increasing the range of motion.
- The procedure is typically performed by orthopedic or joint replacement specialists with advanced surgical techniques.
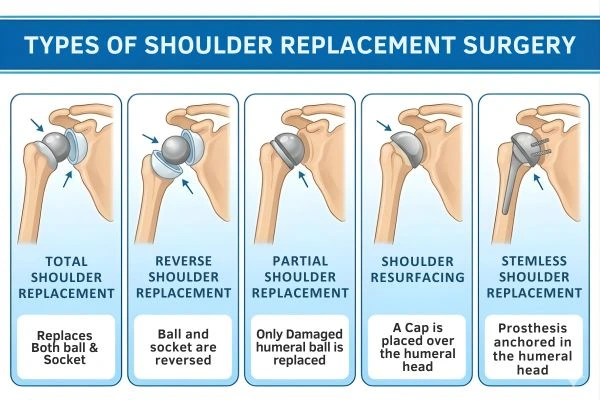
Types of Shoulder Replacement Surgery
-
Total Shoulder Replacement (Anatomic)
Both the ball and socket of the shoulder joint are replaced with prosthetic components. Ideal for patients with intact rotator cuff tendons and severe osteoarthritis. -
Reverse Shoulder Replacement
The position of the ball and socket is reversed to depend more on the deltoid muscle. Suitable for patients with large rotator cuff tears or failed previous shoulder surgeries. -
Partial Shoulder Replacement (Hemiarthroplasty)
Only the ball (head of the humerus) is replaced. Often used when the ball is damaged due to trauma, but the socket is still healthy. -
Shoulder Resurfacing
A less invasive option where only the surface of the humeral head is replaced. Best for younger patients with less joint damage. -
Stemless Shoulder Replacement
A newer technique that avoids using a long metal stem in the upper arm bone. It preserves more bone and may allow easier revision in the future.
Signs You May Need Shoulder Replacement

- Persistent shoulder pain that interferes with daily activities and sleep.
- Limited range of motion in the shoulder, making it hard to lift your arm or reach overhead.
- Weakness in the shoulder, often caused by tendon damage or arthritis.
- Grinding, clicking, or locking sensation in the joint during movement.
- Pain that doesn't improve with medication, physiotherapy, or injections.
- Reduced ability to perform tasks such as dressing, grooming, or carrying objects.
Causes of Shoulder Joint Damage
- Osteoarthritis: A common wear-and-wear condition affecting the cartilage of the shoulder joint. Leads to bone-on-bone contact and chronic pain.
- Rheumatoid Arthritis: An autoimmune disease that inflames the joint lining, causing pain and deformity.
- Post-Traumatic Arthritis: Develops after a shoulder injury such as a fracture or dislocation. Can damage cartilage and lead to early joint degeneration.
- Rotator Cuff Tear Arthropathy: Occurs when massive, long-standing rotator cuff tears result in joint instability.
- Severe Fractures: Complex fractures of the shoulder, especially in elderly patients, may require replacement.
- Failed Previous Shoulder Surgery: Unsuccessful outcomes from earlier surgeries may need revision shoulder replacement.
Benefits of Shoulder Replacement Surgery
- Pain Relief: Most patients experience complete or significant reduction in chronic shoulder pain.
- Improved Range of Motion: Surgery restores mobility, making everyday tasks like combing hair or dressing easier.
- Better Sleep: Reduction in night-time pain helps improve sleep quality.
- Enhanced Quality of Life: Patients can return to light sports, hobbies, and household chores without discomfort.
- Long-Term Joint Function: Implants typically last 10–20 years, providing lasting benefits and independence.
- Boosted Confidence: Restored movement and pain relief help patients regain self-esteem and confidence.
Recovery After Shoulder Replacement Surgery
- Hospital Stay: Usually lasts 1–2 days post-surgery, depending on the type of replacement and overall health.
- Pain Management: Medications and nerve blocks help control pain in the early recovery phase.
- Physiotherapy: Starts within a few days of surgery to regain mobility and prevent stiffness. A progressive rehabilitation plan continues for several weeks to months.
- Activity Limitations: Avoid lifting heavy objects or overhead activities for several weeks. Patients are typically advised to wear a sling for the first few weeks.
- Healing Time: Most patients resume light activities in 6–8 weeks and full function in 3–6 months. Full recovery may take up to a year for optimal strength and flexibility.
Post-Surgery Care and Precautions
- Follow-Up Appointments: Regular check-ups to monitor healing and implant position via X-rays.
- Wound Care: Keep the surgical site clean and dry to avoid infections. Watch for signs of infection like redness, swelling, or discharge.
- Lifestyle Adjustments: Avoid smoking and alcohol to promote faster healing. Eat a healthy diet rich in calcium and protein to support tissue repair.
- Home Exercises: Consistent home-based physiotherapy is crucial to maintaining shoulder mobility. Avoid sudden jerky movements or heavy lifting until cleared by your doctor.
- Long-Term Maintenance: Maintain a healthy weight to avoid joint stress. Periodic reviews help ensure implant longevity and shoulder health.
For personalized care and expert advice, consult with the best Shoulder Surgeon & Sports Injuries Specialist in Mumbai.
If you're dealing with persistent shoulder pain or mobility issues, Dr. Desai offers advanced shoulder replacement surgery options tailored to your needs. To schedule a consultation, feel free to Contact Us today.
FAQs on Shoulder Replacement Surgery in Mumbai
How long does the surgery take?
Shoulder replacement surgery usually takes about 1.5 to 2 hours.
Will I need physiotherapy after surgery?
Yes. Physiotherapy is essential to regain strength, flexibility, and shoulder function.
How long do shoulder implants last?
With proper care, shoulder implants can last 15–20 years or longer.
When can I return to normal activities?
Light daily activities can usually be resumed within a few weeks, as advised by your doctor.
Is shoulder replacement can be done for both shoulders?
Yes. If needed, shoulder replacement can be performed on either shoulder, usually one at a time.